September 10, 2021
Research report: Rehabilitation of COVID-19 patients, a feasibility study
Rehabilitation of COVID-19 patients, a feasibility study
Eva Boomstra MSc1, Karin Gerrits PhD1,2, Femke Piek3, Jaap van Dieën PhD1
1 Department of Human Movement Sciences, Vrije Universiteit Amsterdam, Amsterdam Movement Sciences, Amsterdam, Netherlands
2 Merem Medische Revalidatie, Hilversum, Netherlands
3 Sport-medisch Centrum Kennemerland, Netherlands
Introduction
Many patients with COVID-19 infection experience periods of immobilization after Intensive Care Unit (ICU) admission. These patients have a severely reduced aerobic capacity (1) and in general immobilization at the ICU has been shown to cause what has been coined ICU Acquired Weakness, with associated muscle weakness (2, 3), and cognitive and motor impairments stay (4, 5). More surprisingly, it has recently become apparent that, also in mildly diseased and non-hospitalized patients, COVID-19 infection can cause long-lasting impairments of cardiorespiratory, neuromuscular and cognitive functioning (6, 7). Common symptoms include dyspnea, muscle weakness, fatigue, and cognitive and attentional problems (6, 8, 9). Most patients recover well from a mild COVID-19 infection, but some patients report lasting problems such as fatigue, ‘ brain fog’, difficulty to breathe, also described as ‘Long-Covid’ (11), or post-acute sequelae of COVID19 syndrome (PACS) (10, 11). Estimates of patients with lasting complaints vary from approximately 30% (12, 13), to 20% after 3 weeks and 10% after 3 months (10, 11). In contrast to expectations, patients who have been admitted to the hospital seem to recover more rapidly than patients who suffered from a mild infection at home (13).
Given the poor health status and lasting symptoms after COVID-19 infection, rehabilitation should target cardiorespiratory function and muscle strength and endurance (14), but likely also motor control and cognition. Theory on training and (re-)learning of motor tasks suggests that training should start as early as possible, involve many repetitions, should be task-specific, have an adequate and incremental intensity and should make use of feedback (15).
Motek Medical have developed a training program, for patients recovering from COVID-19 infection, based on published guidelines and these training principles. The training program is incorporated in their HERO Solution (Motek Medical BV, Houten, the Netherlands), which combines a treadmill and three Medical Training Therapy devices all using Virtual Reality applications. All devices are connected with the FysioRoadmap software (Monitored Rehab Systems BV, Haarlem, the Netherlands) which supports treatment planning and facilitates data collection. The program is performed under the supervision of a physiotherapist. It uses treadmill walking as a task-specific training stimulus for mobility and to challenge the cardiovascular and respiratory systems. This is combined with virtual reality (VR) and gaming to provide an additional cognitive challenge. In addition, fitness devices are used to train upper and lower extremity muscle strength, motor control and proprioception. VR and gaming are again employed to provide feedback and to provide additional motor control and cognitive challenges, such as imposed changes in movement speed changes and movement excursions. Exercises are prescribed with incremental intensity, based on current performance, as supported by a protocol integrated in the software. This protocol prescribes standardized assessments, using the same equipment, to assess progress. In addition, continuous monitoring of oxygen saturation is supported, to adjust the intensity of exercise if needed. The project reported here aimed to evaluate feasibility and usability of this targeted rehabilitation program for patients after COVID-19 infection. The program was implemented in a single physiotherapy practice and consecutive patients who consulted the practice for COVID-19 rehabilitation were invited to participate.
Methods
Participants
Nineteen patients (14 females, 5 males, aged 52 (SD 4) years, BMI 28 (SD 1) kg/m2) were included in the study. Exclusion criteria where: not being able to walk, not fit to exercise (according to the ACSM guidelines), no permission from clinician, suspected serious lung problems reported by clinician, not able to understand the instructions. Two other patients were admitted to the program, but dropped out, as they were unable to fit the rehabilitation program in their schedule. Two of the included patients had been hospitalized, seventeen had not been hospitalized. According to their SNAQ+ scores none of the patients were undernourished (all scored > 2).
Clinical evaluation
The intervention was evaluated based on patient reported outcomes and physical fitness tests at baseline and 12 weeks after enrolling in the program. Patient reported outcomes comprised the following items: impairments experienced (Patient Specific Functional Scale (PSFS, (16)), Clinical COPD Questionnaire (17), the shortened Quality-of-Life for Respiratory Illness Questionnaire (RIQ-MON10, (18)), and fatigue and dyspnea at rest and after exertion rated on 10-points Borg-scales (19, 20). In addition, patient satisfaction was measured with the Global Perceived Effect score (21). Physical fitness tests comprised the 6-minutes walk test (22), a sub-maximal cycle test (23), hand grip strength (24), and postural sway during four standing balance tasks (eyes open, eyes closed, tandem stance, unipedal stance (25)).
Usability of the equipment was evaluated with the System Usability Scale (26) filled out by two physiotherapists. In addition, semi-structured interviews on relevance and usability of the program were performed with one physiotherapist and nine patients.
Statistics
Differences between follow-up at 12 weeks and baseline were tested with Student t-tests, when data
were normally distributed, and with Wilcoxon signed rank tests otherwise.
Results
Intervention
The total duration of the program and the number of sessions varied across patients, dependent on progression. The total duration of the program and the number of sessions varied across patients. Dependent on the progress of the patient, their goals and their ability to exercise, the physiotherapist decided (together with the patient) how many sessions were needed to achieve the patient’s rehabilitation goals. On average patients attended 30 (SD 14) sessions at an average of 2 (SD 0.2) sessions per week. Only 13 participants filled out the questionnaires 12-weeks after the program. Loss to follow-up was due to the fact that for some participants the 12-weeks follow-up fell outside of the project period.
Patient reported outcomes
After the intervention, patients experienced less impairments. A significant and clinically relevant difference between baseline and after 12 weeks was found for the Clinical COPD Questionnaire and the RIQ-MON10 (Table 1). In addition, the most impaired activities (PSC activities 1 and 2) showed a significant and clinically relevant improvement (Table 1). The changes in Borg-scores for fatigue and dyspnea after exertion were significant and clinically relevant. The changes Borg-scores for fatigue and dyspnea at rest were, however, not significant.
Table 1: Patient reported outcomes
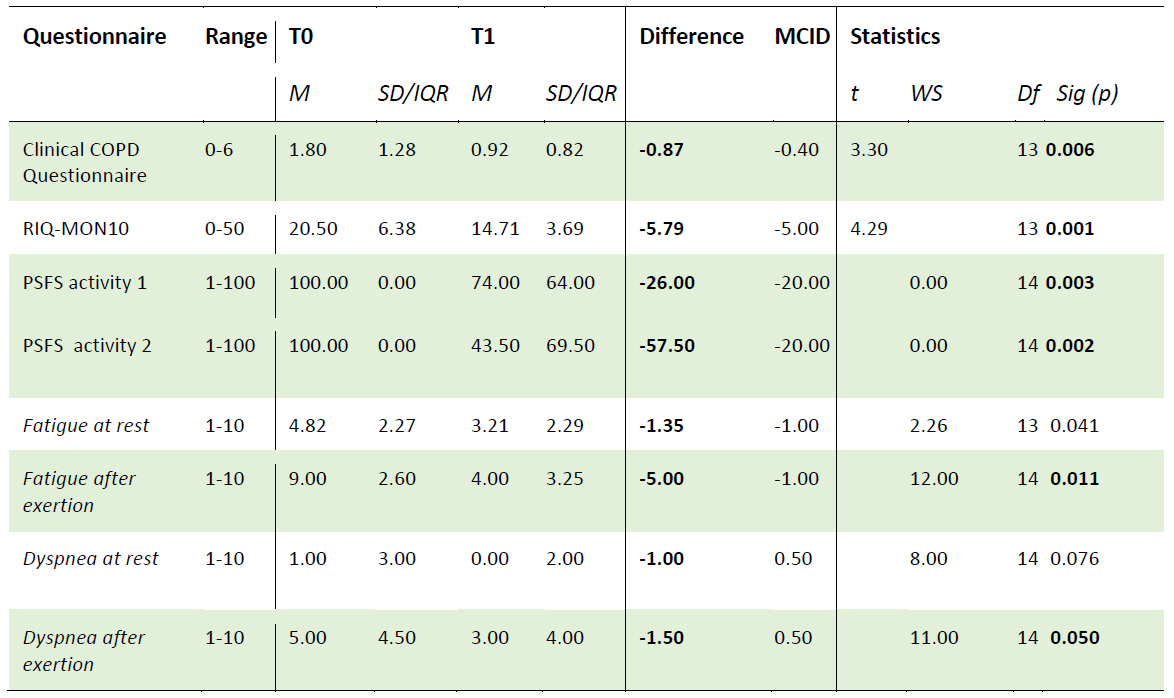
T0 = baseline, T1 = 12 weeks after baseline, M=Mean/Median SD=Standard Deviation IQR=InterQuartile Range, WS=Wilcoxon-Signed Rank Test, df = degrees of freedom Sig=significant. MCID=Minimal Clinical Important Difference. bold = statistically significant or clinically relevant.
The average Global Perceived Effect Scores for recovery and satisfaction were 2.50 (SD 0.67) and 1.62 (SD 0.87), respectively. Scores of 1 (full recovery) and 2 (substantial improvement) are interpreted as clinically relevant.
Physical fitness
The distance covered in the 6-minutes walk test improved with a significant and clinically relevant average effect of 75 (SD 25) m (p= 0.019), but no significant effect was found on the submaximal cycle test (+11 (SD 26) W, p=0.159). Hand grip strength improved significantly, but the effect was lower than the minimal clinically important difference (left +4.50 (SD 6.35) kg p=0.020, right +3.59 (SD 5.25) kg p=0.043.). Postural sway tests were completed in only seven participants. No significant effect was found on the sway path (+0.001 (SD 0.002) cm/s p=0.310).
Relevance
The physiotherapist and patients interviewed considered the program highly relevant. The program was well aligned with the daily routine in physiotherapy care within this practice. While the complaints of the patients varied widely, the program was flexible enough to be adjusted according to their needs. Many of the patients had therapeutic goals related to improving cognition and the program was considered very suitable for this goal. Training on the treadmill with dual tasking was specifically used to this end. Two patients indicated that an additional component aimed at relaxation should be added to the program.
The tests performed were well aligned with the goals of the patients. Balance and gait tests were considered less relevant by both the patients and the physiotherapist. Many patients reached high or maximal scores on these tests at baseline, indicating no impairments in this domain. The physiotherapist and patients missed instrumented tests of fatigue, pacing, cognition and coping mechanisms.
Usability
The physiotherapists rated the equipment as very usable, with an average score of 91% (SD 3%) on the System Usability Scale, where a score of 70% is generally interpreted as good. One patient indicated that the brightness of the screens used was too high. The coupling between the hand grip strength dynamometer and the digital patient record was not adequate at the time of testing, which limited feedback on progress during training. Patients found adherence non-problematic, since the intensity was adjusted based on their status. The frequency of two session per week was considered feasible and not too demanding.
Discussion
This study was performed in a single physiotherapy practice and no control group was used. Obviously, this limits interpretation of our results, but in line with our intentions this study has provided a test of feasibility and usability of the intervention, with positive results. Moreover, it has provided indications for improvement as well as successful features of the intervention which will be discussed below.
Improvements
Based on the patients’ and therapists’ experiences as reported informally and in the interviews, suggestions for improvement of the training and assessment protocol have been formulated. The most limiting factor appears to be endurance and this should be prioritized in therapy. In addition, it is suggested that more attention should be given to cognition and coping. The measurement of oxygen saturation appears redundant as this did not appear to drop in any of the patients and training sessions. Moreover, it may cause patients to rely on measurements rather than respond to their own perception. Measurement of oxygen saturation could be limited to those patients in whom a drop in oxygenation during exercise testing prior to the training program indicates that this is needed. Training and testing of balance appears not to require priority. Similarly gait speed appeared less affected and hence testing (10m walk test) may not be needed. It should be noted, that the lack of problems with balance and speed may reflect that the far majority of participants had not been hospitalized. It would improve feasibility to use shorter or less questionnaires. Malnourishment appears not to be prevalent among the patient group. So, screening could be omitted. Again, this may reflect that the far majority of participants had not been hospitalized.
Success factors
The feedback of therapists and patients also helped to identify success factors of the intervention program. The proposed program allows training of endurance and cognition simultaneously. Patients indicated that this was beneficial to their recovery and encouraged to expand this possibility emphasizing the importance of training of (attention and concentration). The importance of cognitive impairments post-COVID is also emphasized in literature (6). Patients experienced the approach of the therapists and the design of the program as supportive and as an acknowledgement of their problems. This helped them to find a balance between their capacity and the demands of daily life, which was experienced as a major problem that requires not only physical training but also attention to behavioral aspects. Finally, it was considered important that the protocol could be adjusted to the individual patient’s goals.
Conclusions
This project showed that a training program for rehabilitation after COVID-19 infection, based on integrated cognitive and physical training and testing, supervised by experienced therapists, is promising in terms of effects, relevant, and feasible. After the program, we found clinically relevant improvements in impairments and fitness and a clinically relevant decrease in fatigue and dyspnea.
References
1. Blokland IJ, Ilbrink S, Houdijk H, Dijkstra JW, van Bennekom CAM, Fickert R, et al. [Exercise capacity after mechanical ventilation because of COVID-19: Cardiopulmonary exercise tests in clinical rehabilitation]. Ned Tijdschr Geneeskd. 2020;164.
2. Puthucheary ZA, Rawal J, McPhail M, Connolly B, Ratnayake G, Chan P, et al. Acute skeletal muscle wasting in critical illness. JAMA. 2013;310(15):1591-600.
3. Jolley SE, Bunnell AE, Hough CL. ICU-Acquired Weakness. Chest. 2016;150(5):1129-40.
4. Inoue S, Hatakeyama J, Kondo Y, Hifumi T, Sakuramoto H, Kawasaki T, et al. Post-intensive care syndrome: its pathophysiology, prevention, and future directions. Acute Med Surg.
2019;6(3):233-46.
5. Kiriella JB, Araujo T, Vergara M, Lopez-Hernandez L, Cameron JI, Herridge M, et al. Quantitative Evaluation of Muscle Function, Gait, and Postural Control in People Experiencing Critical Illness After Discharge From the Intensive Care Unit. Phys Ther. 2018;98(1):8-15.
6. Amdal CD, Pe M, Falk RS, Piccinin C, Bottomley A, Arraras JI, et al. Health-related quality of life issues, including symptoms, in patients with active COVID-19 or post COVID-19; a systematic literature review. Qual Life Res. 2021.
7. Moreno-Perez O, Merino E, Leon-Ramirez JM, Andres M, Ramos JM, Arenas-Jimenez J, et al. Post-acute COVID-19 syndrome. Incidence and risk factors: A Mediterranean cohort study. J Infect. 2021;82(3):378-83.
8. Huang C, Huang L, Wang Y, Li X, Ren L, Gu X, et al. 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study. The Lancet. 2021;397(10270):220-32.
9. Orru G, Bertelloni D, Diolaiuti F, Mucci F, Di Giuseppe M, Biella M, et al. Long-COVID Syndrome? A Study on the Persistence of Neurological, Psychological and Physiological Symptoms. Healthcare (Basel). 2021;9(5).
10. Pavli A, Theodoridou M, Maltezou HC. Post-COVID syndrome: Incidence, clinical spectrum, and challenges for primary healthcare professionals. Arch Med Res. 2021.
11. Venkatesan P. NICE guideline on long COVID. Lancet Respir Med. 2021;9(2):129.
12. Logue JK, Franko NM, McCulloch DJ, McDonald D, Magedson A, Wolf CR, et al. Sequelae in Adults at 6 Months After COVID-19 Infection. JAMA Netw Open. 2021;4(2):e210830.
13. van den Borst B, Peters JB, Brink M, Schoon Y, Bleeker-Rovers CP, Schers H, et al. Comprehensive health assessment three months after recovery from acute COVID-19. Clin
Infect Dis. 2020.
14. Arena R, Myers J, Ozemek C, Hall G, Severin R, Laddu D, et al. An Evolving Approach to Assessing Cardiorespiratory Fitness, Muscle Function and Bone and Joint Health in the COVID-19 Era. Curr Probl Cardiol. 2021:100879.
15. Kitago T, Krakauer JW. Motor learning principles for neurorehabilitation. Handb Clin Neurol. 2013;110:93-103.
16. Horn KK, Jennings S, Richardson G, Vliet DV, Hefford C, Abbott JH. The patient-specific functional scale: psychometrics, clinimetrics, and application as a clinical outcome measure. J
Orthop Sports Phys Ther. 2012;42(1):30-42.
17. Stallberg B, Nokela M, Ehrs PO, Hjemdal P, Jonsson EW. Validation of the clinical COPD Questionnaire (CCQ) in primary care. Health Qual Life Outcomes. 2009;7:26.
18. Maille AR, Koning CJ, Zwinderman AH, Willems LN, Dijkman JH, Kaptein AA. The development of the ‘Quality-of-life for Respiratory Illness Questionnaire (QOL-RIQ)’: a disease-specific quality of-life questionnaire for patients with mild to moderate chronic non-specific lung disease. Respir Med. 1997;91(5):297-309.
19. Bestall JC, Paul EA, Garrod R, Garnham R, Jones PW, Wedzicha JA. Usefulness of the Medical Research Council (MRC) dyspnoea scale as a measure of disability in patients with chronic obstructive pulmonary disease. Thorax. 1999;54(7):581-6.
20. Williams N. The Borg Rating of Perceived Exertion (RPE) scale. Occupational Medicine. 2017;67(5):404-5.
21. Kamper SJ, Maher CG, Mackay G. Global rating of change scales: a review of strengths and weaknesses and considerations for design. J Man Manip Ther. 2009;17(3):163-70.
22. Butland RJ, Pang J, Gross ER, Woodcock AA, Geddes DM. Two-, six-, and 12-minute walking tests in respiratory disease. Br Med J (Clin Res Ed). 1982;284(6329):1607-8.
23. Chura RL, Marciniuk DD, Clemens R, Butcher SJ. Test-Retest Reliability and Physiological Responses Associated with the Steep Ramp Anaerobic Test in Patients with COPD. Pulm Med. 2012;2012:653831.
24. Hamilton GF, McDonald C, Chenier TC. Measurement of grip strength: validity and reliability of the sphygmomanometer and jamar grip dynamometer. J Orthop Sports Phys Ther.
1992;16(5):215-9.
25. Rossiter-Fornoff JE, Wolf SL, Wolfson LI, Buchner DM. A cross-sectional validation study of the FICSIT common data base static balance measures. Frailty and Injuries: Cooperative Studies of Intervention Techniques. J Gerontol A Biol Sci Med Sci. 1995;50(6):M291-7.
26. Bangor A, Kortum PT, Miller JT. An Empirical Evaluation of the System Usability Scale. International Journal of Human–Computer Interaction. 2008;24:574-94.