January 6, 2020
Clinical integration of the CAREN Extended at Cleveland Clinic

Matt Streicher, Research Engineer
The Center for Neurological restoration at The Cleveland Clinic, Cleveland, Ohio, United States of America.
The Cleveland Clinic is a non-profit academic medical center, that provides clinical and hospital care and is a leader in research, education and health information. The Center for Neurological Restoration at the Cleveland Clinic has assembled one of the nation’s largest teams of dedicated specialists — including neurologists, neurosurgeons, neuropyschologists and specialized nurses, together with physical, occupational, speech and swallow therapists — under one roof to provide truly comprehensive care for patients with any movement disorder. The addition of Motek equipment, such as the CAREN Extended, has allowed our team of therapists and engineers to incorporate this unique experience into daily clinical physical therapy care.

A patient walking on the CAREN system.
Patient Group
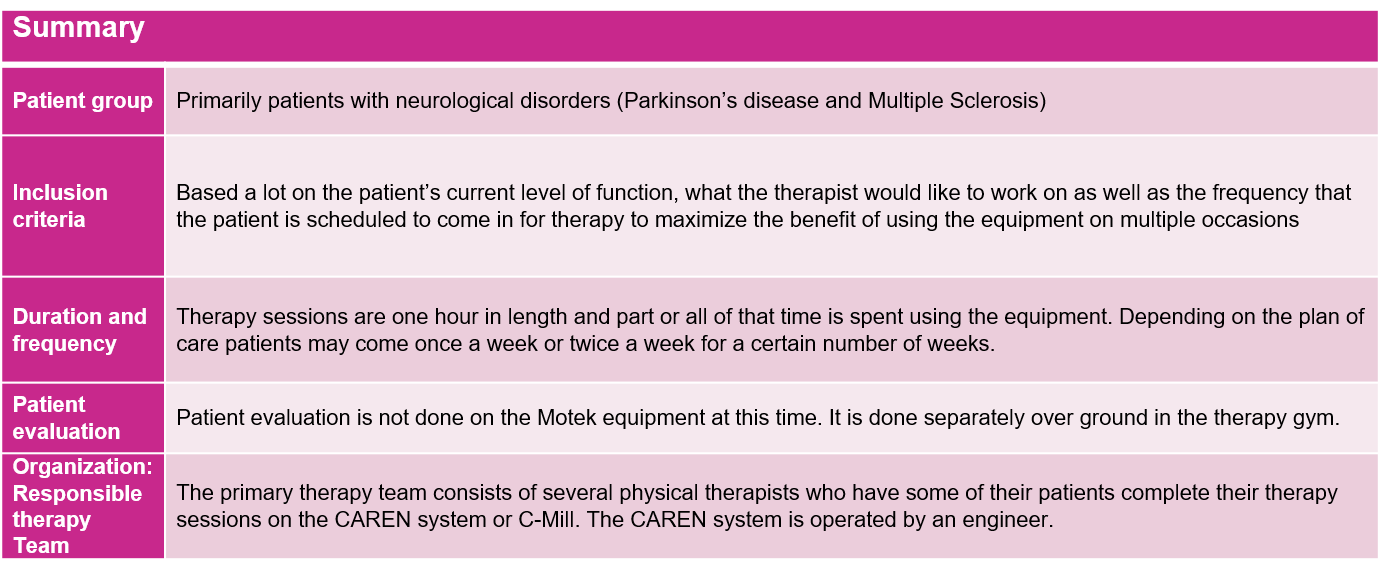
The patients that primarily use this equipment are dealing with some sort of neurological disorder. Most patients have Parkinson’s disease or Multiple Sclerosis but patients with other neurological disorders may be seen as well. Patients get referred to physical therapy by their primary care physician or their specialized neurological doctor. The physical therapist determines whether or not the patient would be a good candidate for therapy using this kind of equipment.
Prescription: inclusion criteria
Physical therapists base their inclusion criteria on the overall severity of the disease and the patient’s current level of function. They also take into consideration what kind of rehabilitation they would like to work on whether it be gait, balance, dual-tasking, etc. In addition, most physical therapists prefer to put patients on equipment like the CAREN system if they are scheduled for multiple future visits so that they can see the full benefit of working with the system as a part of their therapy routine.
Therapists like having the option to be able to use the movable platform dual-task challenges (motor and cognitive). Depending on the availability of the system and on the desired activity, most therapists tend to use the CAREN system for part of the patient’s therapy. For higher functioning patients the CAREN is generally preferred over regular therapy to provide an extra level of challenge for the patient.
Duration and frequency of sessions
Our physical therapy sessions are typically one hour in length. Therapists may bring patients in for part, or all, of their hour-long session depending on their goals for the day or whether or not they need to complete functional assessment evaluations as a part of their therapy. Frequency of sessions depends on the individual care plan as well as the patient’s insurance coverage. Some patients come once a week or every other week for a few months, while others may schedule intensive training coming twice a week for one month and then do that every three to four months during the calendar year. The CAREN system is split 50/50 between research and physical therapy which sometimes limits the amount of access the physical therapy department has to the system. The research projects conducted using the CAREN include:
· Evaluation of the effect on gait of single and multi-modal training in people with Parkinson’s (Rosenfeldt A.B. et al 2019[1]).
· Evaluating the feasibility and effects of virtual reality vs. traditional physical therapy in multiple sclerosis patients (Streicher M.C. et al 2018)[2].
You can read more about this study here and more about other studies using the CAREN Extended, including those at the Cleveland Clinic, here.

Patient evaluation
Patient evaluation occurs on the initial visit and at the last visit of their therapy program to understand the benefits of the treatment. Typically evaluations are done once a month to gauge overall progress. Evaluations are not done with any of the Motek devices though. Therapists complete their evaluations separately in the therapy gym with assessments such as BERG Balance, six-minute walk, Timed Up & Go, etc. Therapists prefer walking tests to be done overground instead of on the CAREN because the learning curve for self-paced walking can be difficult for some patients, especially for those with cognitive impairments. Depending on the individual care plan, some patients will schedule for future physical therapy appointments in three to six months as a check-up evaluation or another intensive month’s worth of therapy.
What are the main reasons to include Motek technology as part of the therapy?
Using Motek technology as a part of physical therapy provides a more engaging atmosphere while the patient is going through their therapy or rehabilitation. The ability to provide instantaneous feedback significantly helps patients and therapists during their therapy sessions. Additionally, the CAREN system allows the patients who are at a higher level of function to be challenged. We commonly use the system for dual task challenges and the movable platform will challenge the patient’s balance or gait on a moving surface. This kind of technology presents the opportunity to experience more real-world type environments or more difficult situations that may be helpful in everyday life outside of the therapy world.
Organization: responsible team
Our staff includes seven PTs, two OT’s, one SLP, one biomechanical engineer, and one Patient Service Specialist. The therapy staff has over 154 years of total rehab experience! Mellen Neurorehabilitation had nearly 7000 patient visits in 2018!
[1] Rosenfeldt, A. B., Penko, A. L., Streicher, M. C., Zimmerman, N. M., Koop, M. M., & Alberts, J. L. (2019). Improvements in temporal and postural aspects of gait vary following single- and multi-modal training in individuals with Parkinson’s disease. Parkinsonism & Related Disorders. doi:10.1016/j.parkreldis.2019.05.021
[2] Streicher M.C., Alberts J.L., Sutliff M.H. & Bethoux F. (2019) Effects and feasibility of virtual reality system vs traditional physical therapy training in multiple sclerosis patients. International Journal of Therapy and Rehabilitation doi.org/10.12968/ijtr.2018.25.10.522